
Polycystic ovary syndrome (PCOS), is a common endocrine-metabolic disorder, that was previously, poorly understood. Today, evidence suggests that hyperinsulinemia (elevated levels of insulin hormone) is the underlying cause of PCOS.
Recent estimates suggest a 15-20% prevalence in women, with up to 75% of individuals being undiagnosed. Lack of awareness and discussion about PCOS has resulted in it being the most common cause of infertility.
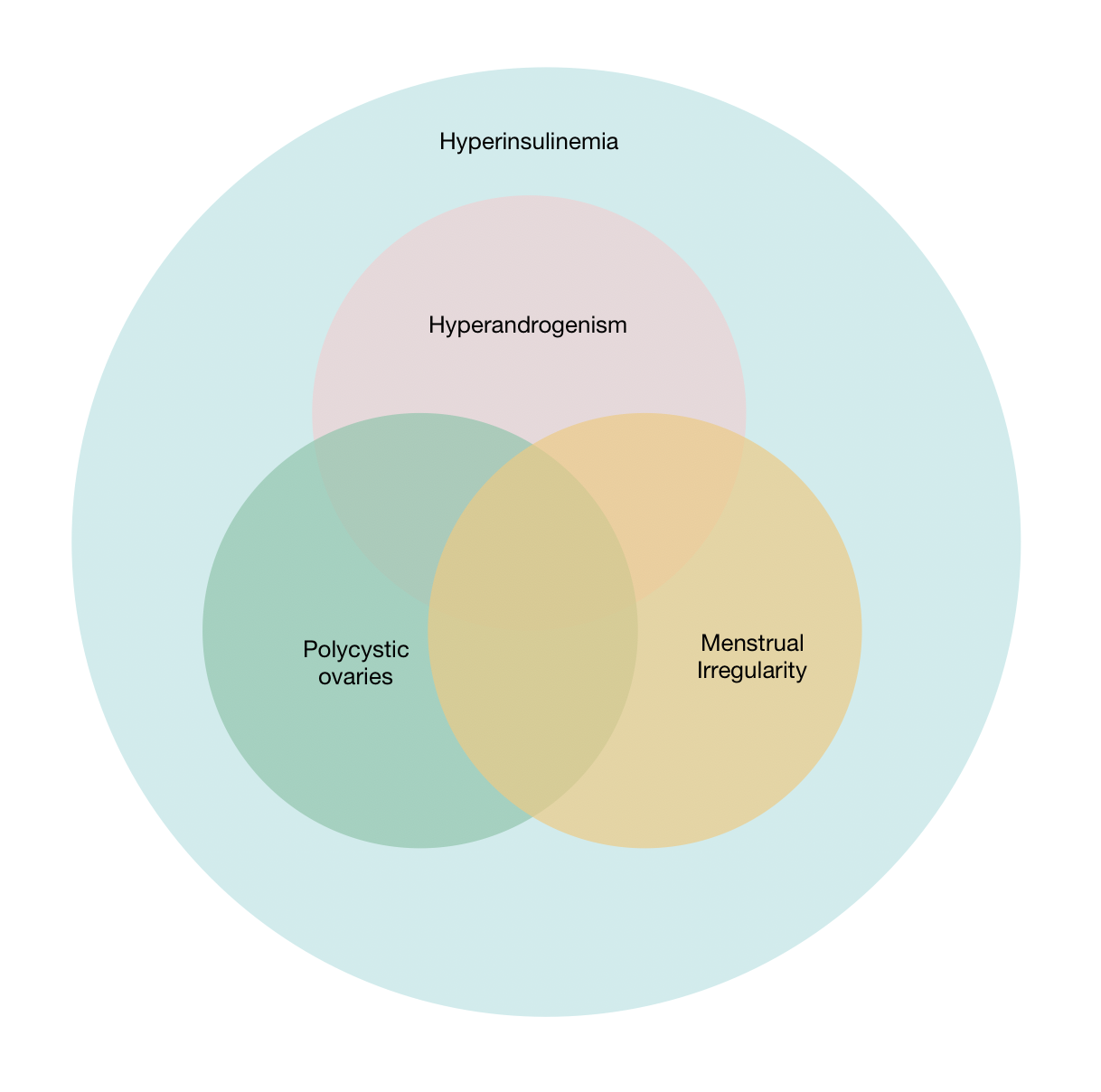
1. Hyperandrogenism — elevated levels of male hormones, namely testosterone
2. Irregular periods — heavy or missed periods
3. Polyctystic ovaries —despite the name, these are not cysts, rather small fluid filled sacs in the ovaries.
A person is diagnosed with PCOS if they present with two or more of these characteristics. Despite the name, an individual can have PCOS even if they don't have polycystic ovaries.
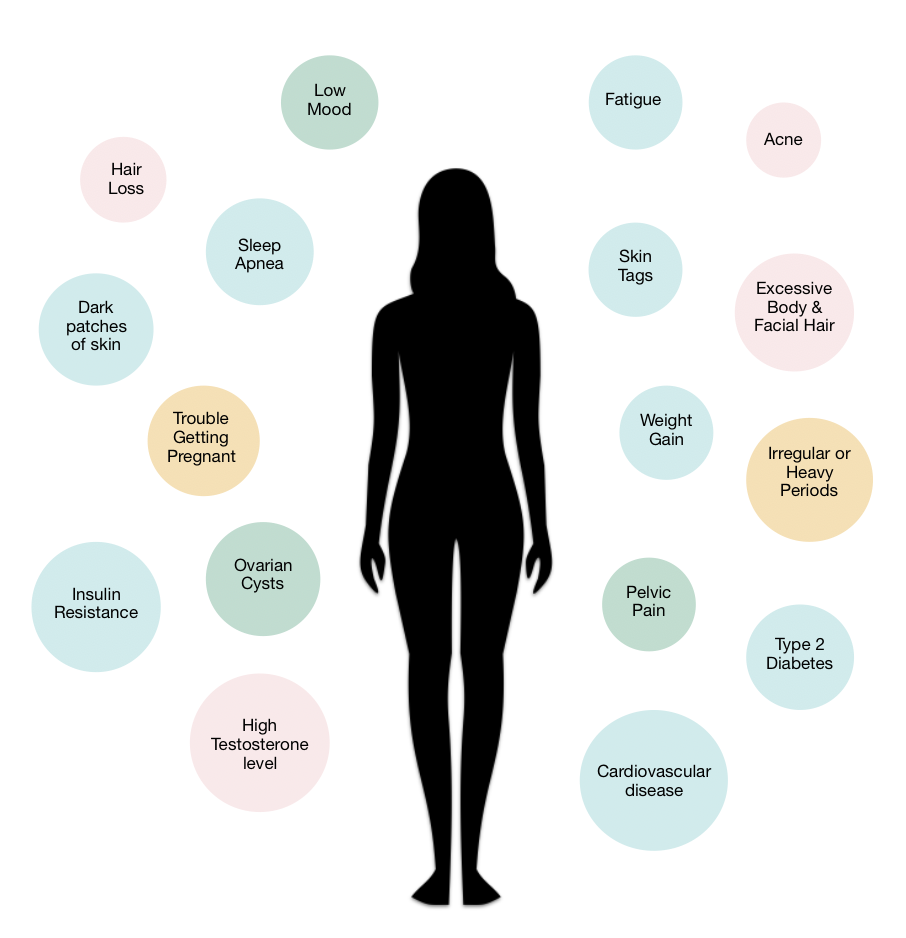
There are various symptoms for PCOS, and some are more obvious than others. For this reason, PCOS can often go undiagnosed or misdiagnosed.
Physical features of PCOS include excess body and facial hair (chin, upper lip, chest and back), hair loss, skin tags, dark–velvety patches of skin, acne, unexplained weight gain, pelvic pain, irregular or heavy periods, fatigue and low mood. These symptoms can be easily identified, but often brushed off as 'normal' or 'part of your make-up' — they are not always normal and should be checked out.
PCOS is not always visible to the naked eye. Your doctor will be able to preform necessary tests to investigate other symptoms of PCOS including elevated hormones (insulin, testosterone, luteinising hormone, and cortisol), insulin resistance and ovarian cysts.
And the story doesn't end there. PCOS can also increases the risk of developing other health conditions like type 2 diabetes, obesity, non-alcoholic liver disease, cardiovascular disease, infertility, depression and sleep apnea (irregular breathing during sleep).
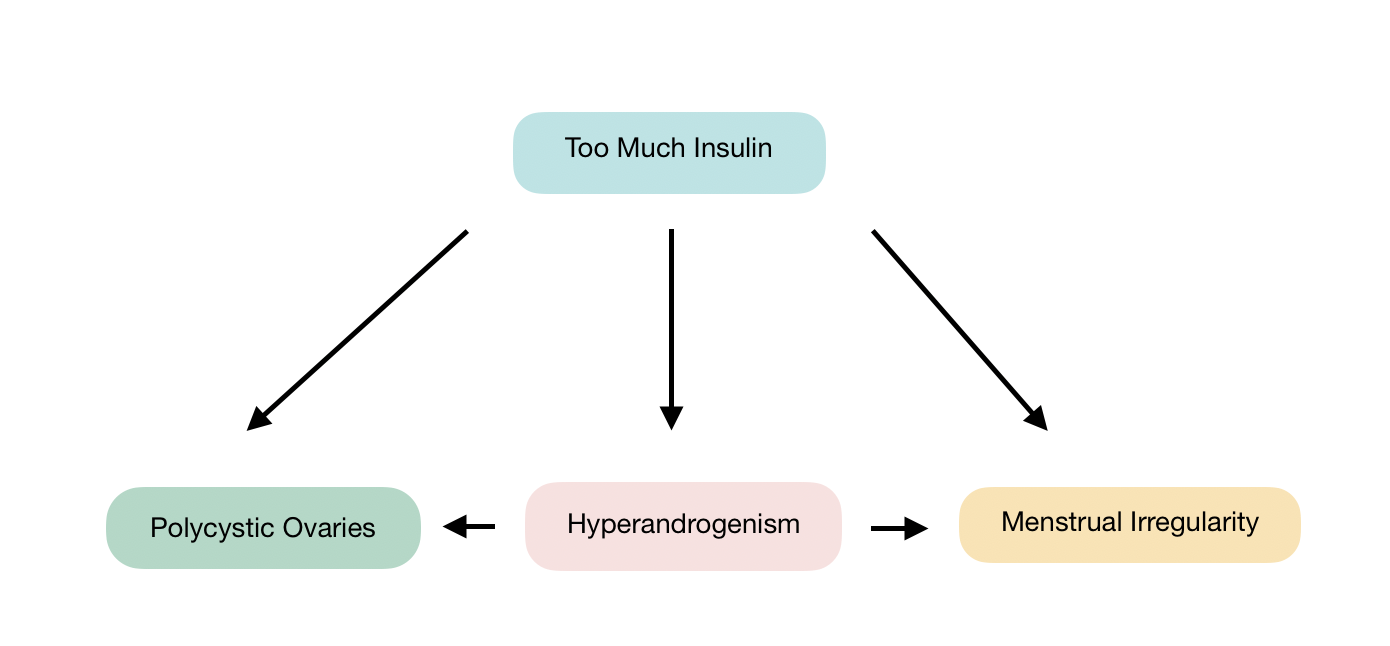
The body is finely tuned by a delicate, complex system of hormones. Working together in harmony, they keep our body balanced. Disrupting just one of these hormones can throw the whole body into disarray. This is exactly what happens with PCOS.
High levels of the insulin (hyperinsulinaemia) rattles the normal functioning of other hormones, which causes a constellation of symptoms.
Let's take a closer look at how hyperinsulinemia contributes to the three main features of PCOS : hyperandrogenism, irregular periods and polyctystic ovaries.
Androgens are commonly known as 'male hormones', like testosterone. Females naturally have androgens, just in smaller amounts to men.
Hyperandrogenism is when an individual has higher than normal levels of androgens, which can cause masculinizing features like male pattern baldness, excess body and facial hair, acne and disrupted periods — this is largely due to elevated levels of testosterone.
In women, testosterone is synthesised in the ovaries and adrenal glands (two glands sitting on top of the kidneys). Studies have shown that the ovaries are the main source of elevated testosterone in PCOS.
Hyperinsulinemia contributes to hyperandrogenism in two ways — it stimulates overproduction of testosterone in the ovaries and down regulates SHGB (sex hormone-binding globulin) synthesis in the liver.
SHGB transports inactive testosterone around the body — free testosterone is active and effects surrounding tissue. The combination of high testosterone and low SHGB intensifies testosterone's effect on the body, causing masculine features.
A normal menstrual cycle is orchestrated by a symphony of hormones that rise and fall in tune with each other. At the beginning of the cycle, a hormone called FSH (follicle stimulating hormone) prompts the ovaries to develop a few follicles, which contain immature eggs — we call these primary follicles.
Testosterone dictates the number and growth of primary follicles. The biggest, most developed primary follicle is selected and triggers the rest of the follicles to die away.
Around the middle of the cycle, a surge of LH (luteinising hormone) signals the follicle to release the mature egg from the ovaries — ovulation occurs.
The egg travels down the fallopian tube, in the hope that it will meet sperm and be fertilised. In the meantime, the empty follicle secretes oestrogen and progesterone, which develops the lining of the womb to support pregnancy.
If the egg is not fertilised, then the lining and egg is shed from the uterus — this is the beginning of the menstrual cycle; a period. Hormones work in perfect sync with each other; it's like Mozart.
However, with PCOS, things don't run so smoothly. Working directly and indirectly, insulin interferes with the delicate balance of FSH/LH and puts everything out of tune.
We know that insulin drives testosterone, and testosterone is closely related to the number of primary follicles produced at the beginning of menstrual cycle. High testosterone can cause up to a 6 fold increase in the number of primary follicles.
Adding fuel to the fire, insulin has been shown to influence hypersecretion and sensitivity of LH. The immature primary follicles are stimulated by LH, but none of them are developed enough to be picked 'as the chosen one' for ovulation. Ovulation doesn't occur, and this has a knock on effect to the rest of the cycle.
The immature follicles have no stimulus for 'die off' so they remain in the ovary and fill with fluid, creating many sacs — this is what we know as polycystic ovaries.
In the absence of ovulation, there is neither an egg to be fertilised, nor am empty follicle to prepare the lining of the womb (stimulated by oestrogen and progesterone). This causes irregular bleeding and infertility.
As discussed, the central pathogenesis of PCOS is hyperinsulinemia. To reverse PCOS, you must treat the root cause of the condition; hyperinsulinemia.
Certain factors like a carbohydrate rich diet, stress, sedentary lifestyle, poor sleep, overeating, snacking, and medication are well known to increase insulin.
Diet and lifestyle changes, that reduce insulin, will ultimately restore hormones and heal PCOS. This can be achieved with a low carbohydrate diet, intermittent fasting, reducing stress and increasing exercise.
Studies have shown that a low-carb diet alone, is an effective, non-invasive treatment plan to reverse PCOS, and remove medication, like clomifene and metformin.
A low carbohydrate diet is a simple solution to a complex syndrome that will help woman regain emotion-physical wellbeing, and avoid devastating complications of infertility.
We now understand more about PCOS, and how to treat it holistically. This is half the battle. We need to start talking about PCOS as a reversible condition.
I encourage you to chat openly with your friends and family about female health — even males; trust me, they're as curious as we are about workings of the female body!
Spread the word so that we can help the 75% of women who are left undiagnosed and silently suffering with cruel symptoms of PCOS — let's make babies!
Stay tuned for more guides, to help you with your health journey.
Take care 👋
Rachel
I’m sure you’re curious about the science behind all this 🔬 Here are some recent medical publications about this topic:
https://academic.oup.com/humrep/article/33/9/1602/5056069
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1334192/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5372867/
https://www.ncbi.nlm.nih.gov/pubmed/23315061
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4334071/#B4
https://www.ncbi.nlm.nih.gov/pubmed/9408743
https://www.mdpi.com/1660-4601/15/11/2589/htm
https://insulinresistance.org/index.php/jir/article/view/50/184#CIT0001_50
https://www.ncbi.nlm.nih.gov/pubmed/12827388
https://www.ncbi.nlm.nih.gov/pubmed/9618791