

A blood glucose measurement is a biomarker, used for diagnosing diabetes and monitoring blood glucose control. This guide will help you understand blood glucose measurements and so that you can evaluate your metabolic health and make necessary lifestyle changes to push diabetes into remission. 💪
A blood glucose measurement is the amount of glucose in the blood at a particular time point. Blood glucose levels are variable. They will rise and fall depending on the time of day and influence of exercise, food, stress, hormones, fasting and medication.
In response to this, hormones called insulin and glucagon regulate blood glucose levels within a narrow range to maintain homeostasis. This range is optimally between 4.0–7.8 mmol/l (72–140mg/dl).
Blood glucose can be tested a few ways — using glucometer, continuous glucose monitoring (CGM) and a fasting plasma glucose test. Glucometers and CGMs are easy to use home tests that can be used at any time point to monitor blood glucose level.
To use a glucometer, a small drop of blood is drawn using a small, sharp needle (called a lancet), and applied to a test strip (already inserted into the glucometer). The glucometer will calculate blood glucose measurement in about 10–20 seconds.
A CGM is inserted under the skin and measures interstitial glucose continually for about 14 days. The time delay between interstitial glucose and blood glucose is approximately 9 minutes, ie. CGM measurement at a single time point will reflect true blood glucose levels around 9 minutes earlier.
A fasting plasma glucose test is carried out by your doctor who will draw a sample of blood, after at least 8 hours fasting. The blood sample is sent to a lab for analysis and your results will be reported by your surgery. This is normally done as a routine check-up or to diagnose diabetes.
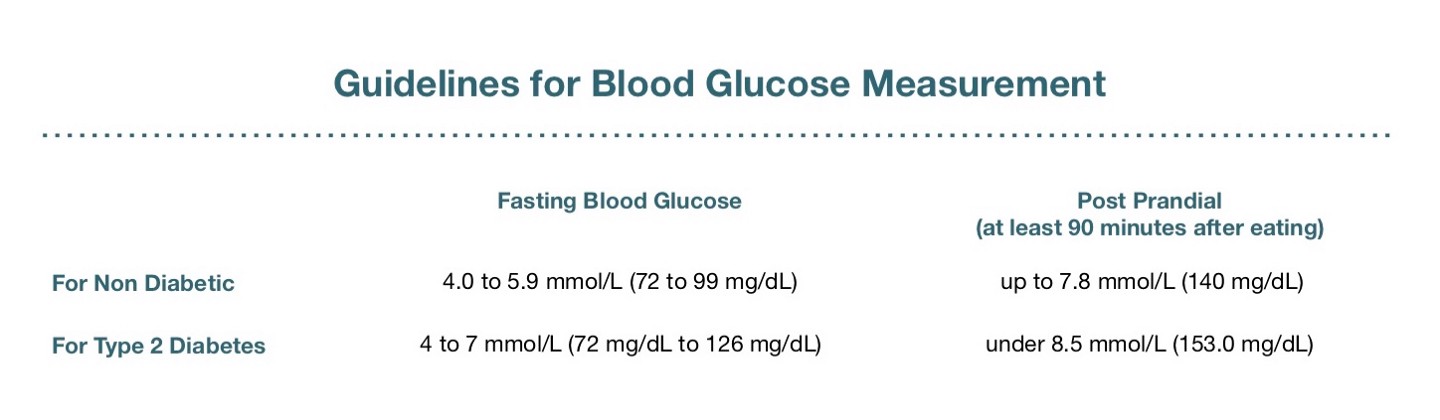
A normal blood glucose result will vary between individuals. Your personal blood glucose target will depend on whether or not you have prediabetes or type 2 diabetes, and where you are in your health journey.
If you have been diagnosed with prediabetes or type 2 diabetes and in the initial phases of diet changes, then blood glucose targets for type 2 diabetes are more appropriate.
If you are a non-diabetic or have reversed insulin resistance, aim for non-diabetic glucose levels. Non-diabetic blood glucose levels should be the ultimate goal for everyone, however there are certain situation that make this more difficult — if beta cells have been damaged and you can’t produce enough insulin.
Fasting blood glucose is measured after 8 hours of fasting, usually in the morning before the first meal of the day. Between 1–2 hours after eating, blood sugars will rise — this is called post prandial blood glucose. Two hours after eating, blood glucose levels will fall again and should reach within fasting blood glucose range
Testing with a glucometer is an easy and effective way to get instant feedback on how diet, lifestyle and medication are effecting your blood glucose. This information is necessary for creating a treatment plan to normalise blood sugars and improve insulin sensitivity. We encourage you to test blood sugars as much as possible, especially in the beginning. This will give you a comprehensive understanding of your personal metabolic health and how to improve it. Once you’ve reached target blood glucose levels, you won’t need to test as much as you’ll have developed an understanding of how to keep blood sugars within normal range. Below are some suggestions for when to test blood glucose.
If you can only make one measurement per day, make it your morning fasting blood glucose. Record this baseline value daily. This will give you an insight into your average blood glucose level and clearly illustrate whether your blood glucose levels are trending upward or downward. With this information you can monitor disease progression or regression and make any suitable adjustments to diet, exercise or medication.
Please note that the dawn phenomenon can cause high morning fasting blood glucose levels. This can be alarming, but it is a normal physiological response that will get better with time and improved insulin sensitivity.
You may like to use your glucometer to ascertain your personal glucose tolerance and to help identify what foods do or don’t raise glucose. This is a simple but powerful technique that is often referred to the “eat to your meter” method — check blood glucose before meal, again 90 minutes after eating and observe results.
It is a process of trial, error and elimination of food, as you gain an understanding of how your body responds to certain food — what and how much can you eat, without raising your blood sugars. A low-carb diet is a brilliant blueprint for lowering blood glucose, however, we are all different and have a unique response to foods. For me, black coffee raises my blood sugars, but if I add cream or have it with a meal, my blood sugars remain stable. This will be different for someone else, and the only true way of knowing how to fine tune your diet is to keep testing pre and post prandial blood glucose.
If the meal has caused a considerable spike at the 90 minute mark, or your levels have remained elevated at 4 hours, you may need to remove, or adjust portion size of this meal.
Your aim is to get your blood sugars within a normal target for either diabetic or non-diabetic (refer to blood glucose targets above), depending on where you are with your health journey.
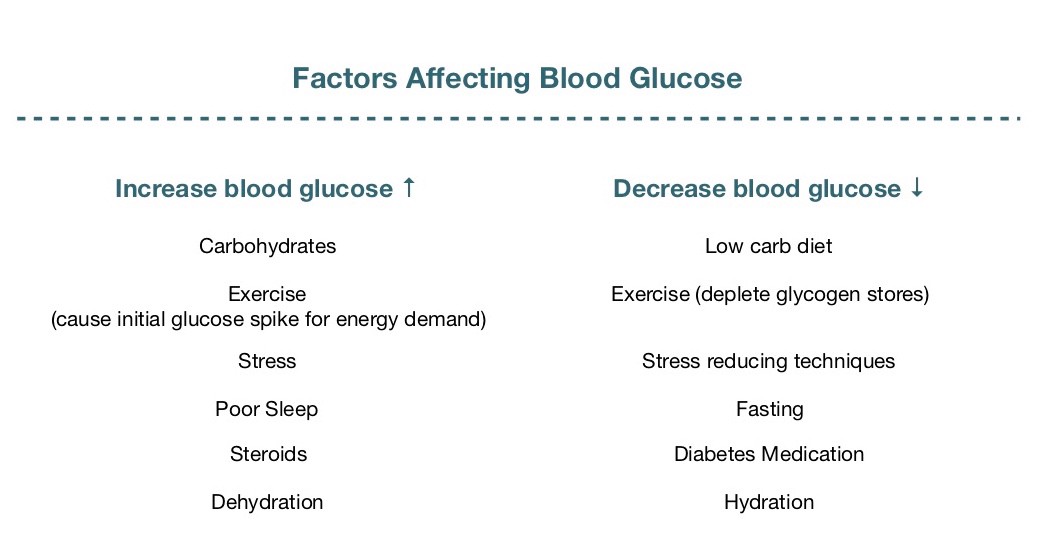
Over the long term, exercise will deplete glycogen stores and improve insulin sensitivity. However, exercise can pose challenges with blood sugar control and result in dangerous fluctuations in hypo and hyperglycaemia.
You may have noticed that during or after exercise, there is a temporary rise in blood glucose. This is because exercise promotes acute stress and increases energy demand. As a result, hormones like adrenaline and cortisol are released which signals the liver to dump glucose into the bloodstream. Your muscles use this glucose for energy to fuel exercise. If you are insulin resistant, it will take longer to clear this ‘dump’ of glucose into the blood stream so you may notice a significant rise in blood glucose that remains elevated for some time. If you are taking medication, low blood glucose can also be a concern as muscles readily draw on stored and circulating glucose for energy.
Monitoring blood glucose before and after exercise will allow you to adjust your exercise regime and medication appropriately so that you can maintain blood glucose within a safe limit.
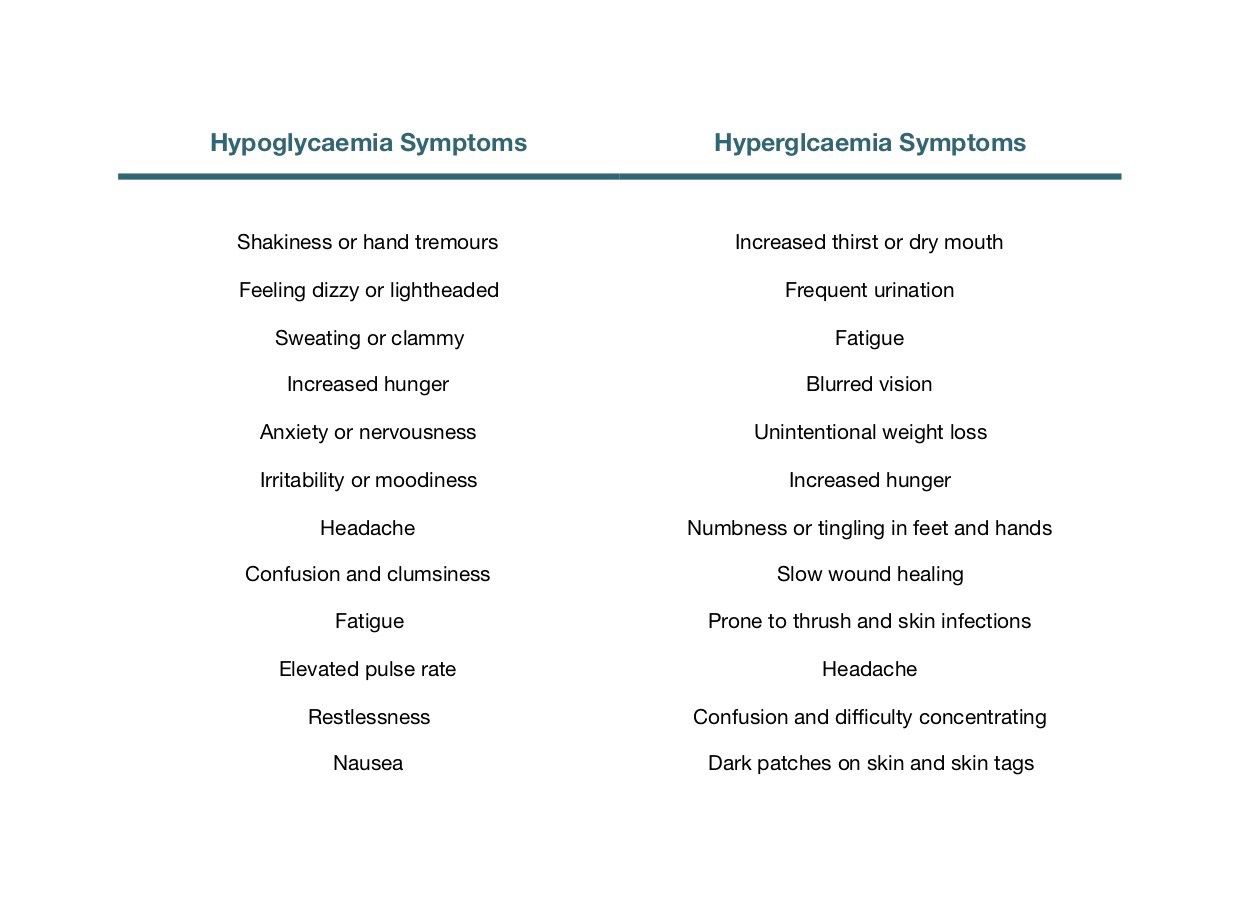
Check your blood sugar if you experience any hypo or hyperglycaemic symptoms. For a person with diabetes, a level below 3.9mmol/l (70mg/dl) is considered hypoglycaemic. Symptoms for hypoglycaemia are normally sudden as the body tries to quickly regain homeostasis.
Hyperglycaemia will normally present with symptoms when blood glucose is higher than 10mmol/l or 180mg/dl. Symptoms will normally develop slowly over a number of days, weeks or months, depending on how long blood glucose has been elevated.
Blood glucose that is either too high or too low can be very dangerous, so it is important to test and contact your doctor if you experience any of the symptoms below.
If you ever have a high or low blood glucose reading, try to problem solve with your doctor and understand why your blood glucose is out of range, so you can prevent it from happening again.
If blood glucose is going too low, you will most likely need to adjust medication. If blood glucose is too high, you may need to adjust diet, medication and exercise.
Fasting blood glucose fluctuates for a number of reasons, even on a low-carb diet. It’s important to bear this in mind when testing blood glucose so that you can understand highs and lows and make necessary changes to bring them back within normal range. If you experience high blood glucose, use the list below to help pin point the reason for this. You can then look at ways to decrease blood glucose — low carb diet, exercise, stress reducing techniques, better sleep, fasting, medication and hydration.
Blood glucose testing is not just for diabetics. It’s an essential tool that everyone should have in their back pocket to help monitor health. I urge you to test as much as possible so that you can establish trends and reveal insights into your metabolic health. We’re all individuals, at different stages of a health journey, and with a unique glucose tolerance to food. The only way to discover what works best for you is to test, and keep testing! This will provide instant results, specific to you, so that you can adjust diet, lifestyle or medication to achieve your health goals.
Stay tuned for more guides, to help you with your health journey.
Take care,
Adam
I’m sure you’re curious about the science behind all this 🔬 Here are some recent medical publications about this topic:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4667340/
https://clinical.diabetesjournals.org/content/36/2/202
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3920802/
https://professional.diabetes.org/sites/professional.diabetes.org/files/media/abridged_standards_of_medical_care_in_diabetes_2017_0.pdf
And a book that is well worth reading...
Diabetes Solution by Dr. Richard K. Bernstein